Trust in white coats has dropped from 71% in 2019 to 40% in 2024, but it’s still undeservedly too high. This is a long but fascinating article from a white coat. The interesting bit to me is how they harmed and wiped out so many white coats and nurses with the gene therapy, which I think is purposeful. The whole push is to less qualified people like the nurse practitioners talked about below, who will consult with you via video call and prescribe you the latest high profit pharmaceuticals, to be delivered to your door. There was a recent survey that reported 61% of people on some type of pharmaceutical, but really people are usually on multiple, with most not needed and actually harmful. The wife had a coworker given a pharmaceutical she didn’t really need that destroyed her kidney, now with a kidney transplant and on immune suppressing drugs for life, and you still have to redo the transplant after so many years as your immune system destroys it. White coats will Merck you if you let them.
https://pierrekorymedicalmusings.com/p/two-texas-girls-dead-one-system-failing
I am disturbed by the increasing failure of today’s doctors, advanced practice providers, and nurses to deliver high-quality, competent, and error-free care. Here, I explore disturbing data trends.
Pierre Kory, MD, MPA

Let’s start by recalling the article below published in JAMA in July of 2024 by researchers at Mass General (Haavaad), where they reported that “trust in hospitals and doctors” plummeted from 71.5% in 2019 to only 40% in 2024:
Mainstream media published several articles in response to the study, where they tried to come up with explanations for the plummeting trust. My favorite obfuscation was this US News World Report article, whose headline read:
“Some Americans?” How about A TON of Americans? In 4 years, trust slipped from 71% to 40%. That ain’t “some.” The most honest and revealing sentence was a direct recitation of the findings in the paper:
”People who trusted medicine less tended to question the financial motives of doctors and hospitals, doubt the quality of care, suspect that care was being influenced by other entities or agendas (Ed: conspiracy theorists!), or perceive discrimination or bias (Ed: like towards the unvaccinated?).
In this APHA article, the journalist tried to blame “us” for the loss of trust, i.e., those who publicly called out the corrupted and unscientific policies in COVID-19:
“Medicine became highly politicized in COVID due to ‘misinformation being amplified by public figures, including some physicians (Ed: moi? oh no!) and the President.
Elected leaders and popular personas encouraged people to doubt science and disregard public health advice “aimed at protecting their health.”
I am about to throw up here. Recall that the new head of the FDA, Dr. Marty Makary, testified in a Congressional hearing that “the biggest purveyor of misinformation during Covid… was the government.” Yet the APHA blames me and others instead of captured government agencies and officials working in the service of the criminal syndicate otherwise known as “Big Pharma.”
Am I being grandiose in thinking I was personally being referred to in that article? Sadly, no. In the below JAMA article (look at the title), they analyzed the biggest physician purveyors of misinformation on social media, and a number of my tweets showed up (red circles):
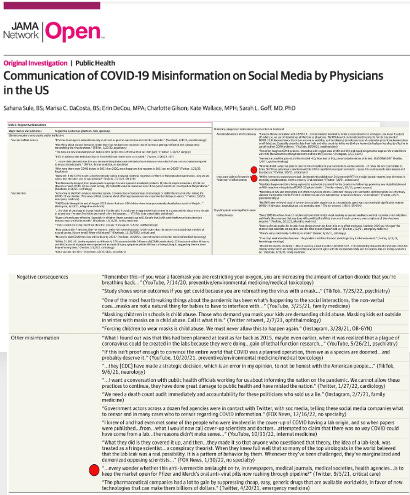
If you can’t read my tweets above, here they are:
… ever wonder whether this anti-ivermectin onslaught on TV, in newspapers, medical journals, medical societies, and health agencies… is to keep the market open for Pfizer and Merck’s oral anti-viral pills rushing through the pipeline?
Umm, how is that misinformation? I was just asking a question! Another one:
Attorney Ralph Lorigo has gone to court to force hospitals to give ivermectin to ventilated patients… 12 times. He won court orders 11 times. Nine of those patients are home; the 10th is recovering rapidly. I guess this country needs more lawyers and fewer doctors.
Clever tweet, right? That was also factual and not misinformation. One of the saddest datasets in Covid was Ralph’s ultimate track record in those lawsuits, which I covered in a chapter called “A Legal Legend” in my book, “The War On Ivermectin,” and will repost here again:
Ralph received 200 consultations to sue hospitals for patients being denied ivermectin. Eighty went to court. He won 40 and lost 40 (the hospitals started heavily lawyering up, and the judges began turning on him, especially in blue districts). Of the 40 he won, 38 survived. Of the 40 he lost, two survived.
Could you let that sink in for a second? Like the “measles cases,” that data still enrages me (literally) to this day. Here is yet another tweet of mine that the study authors categorized as “misinformation”:
“WHO’s ivermectin research team lead…independently publishes on 24 ivermectin RCTs in a major journal—reports large decreases in mortality, hospitalization, time to recovery, viral clearance.”
Again, this is a 100% true statement (at least until that same WHO team lead, Dr. Andrew Hill, later “self-retracted” the paper, threw out a number of the trials originally included, and then re-analyzed it as negative for mortality). Important context: Hill depends on grant funding from major national and international health care organizations for a living.
The comic relief of the JAMA paper is when the authors provided their definitions of what constituted misinformation in COVID-19. Try not to laugh:
The virus was concocted in a lab (Ed: true), natural immunity is equal or better than vaccine immunity (Ed: true), ivermectin and hydroxychloroquine are effective (Ed: true), the vaccines are ineffective, toxic and lethal (Ed: true, true, and true), that federal agencies were working directly in the service of Pharma (Ed: true but I would also include the Dept. Of Defense as well).
Clown world. The article then ends in typical fashion: “Further research should delve into understanding the lack of trust in doctors and hospitals, the researchers suggested.”
As you can see from the above, the media articles that covered the study made little serious or honest attempt at identifying the true causes of the loss of trust. Here are mine (note this list is not meant to be comprehensive, just a “top ten”):
- The pandemic outbreak was met with immediate attempts by public health leaders (Fauci) to cover up the fact that the virus was engineered in a bioweapons lab funded by the U.S.
- The disturbing contradiction of policies that locked down small businesses and churches while allowing big box retailers and liquor stores to remain open
- Wanton issuing and enforcement of non-scientific policies like 6-foot distancing and ubiquitous masking without assessing efficacy and then ignoring obvious adverse downstream effects (like loss of IQ in children)
- Mass media and health agencies’ “gaslighting” of the public by ignoring and censoring the massive rates of vaccine injuries being reported
- Incessant and brazen manipulation and/or “cherry-picking” of data by officials, journals, and agencies to convince the public of the safety and efficacy of the vaccines
- Mandating and/or coercing the most dangerous medical intervention in history by taking away people’s livelihoods and/or freedom to travel if they refused.
- Designing, conducting, and publishing trials that were manipulated to show that ivermectin and hydroxychloroquine (and others) were ineffective and/or dangerous (which then fueled negative corporate media public relations campaigns).
- Using “lawfare” against doctors prescribing “off-label” treatments via persecutory actions by the FDA, Medical Boards, Pharmacy Boards, and Specialty Certification Boards (which in turn, also scared pharmacists from filling the prescriptions).
- Enforcing rigid adherence to largely ineffective, dangerous, and highly remunerated hospital protocols centered around the use of remdesivir and artificially lowered doses of corticosteroids, all of which led to a massive amount of deaths compared to other countries.
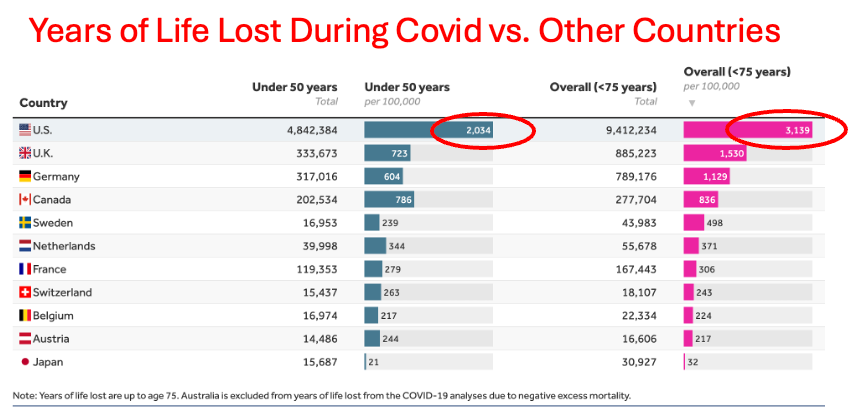
The culmination of all of the above policies in the U.S:
DETERIORATING QUALITY OF CARE IN AMERICAN MEDICINE
My next question is whether, in addition to the reasons I gave above for the loss of trust, how much of it is also being driven by a deterioration in the quality of care in U.S hospitals?
I have over 15 years of experience reviewing law firms’ medical malpractice cases. In my review of the medical records of Daisy Hillebrand and Kaley Fehr (the two girls in Texas who died of inept medical care, not measles), I found unprecedented missteps, errors, incompetence, and a lack of critical (or clinical) reasoning skills. The abysmal care I witnessed led me to question whether there has been a significant drop in the quality of care in the U.S.
Lo and behold, I quickly discovered that the quality of care in the U.S has deteriorated rapidly compared to other countries, timed with the onset of the pandemic. The data below was sourced from the non-profit organization Peterson-KKF Health’s System Tracker, where I found the following:
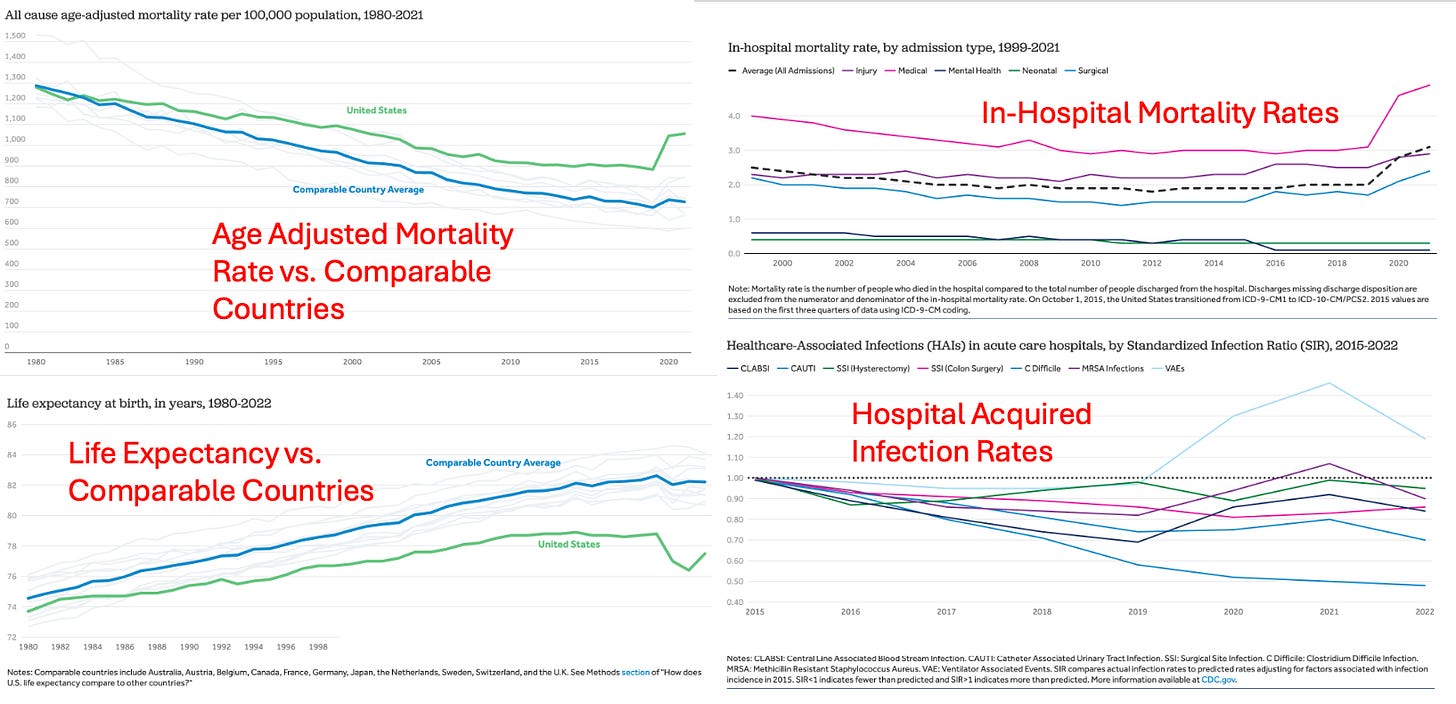
As you can see above, since 2019, the quality of medical care in the United States has resulted in pronounced increases in in-hospital mortality (for injury, surgical, medical, and especially mental health), age-adjusted mortality, and hospital-acquired infections, while life expectancy has plummeted. The latter finding is one of the most disturbing because it can only be caused by sudden rises in deaths among the young (older adults dying cannot impact average life expectancy as drastically).
A commenter on my prior post reviewing the two records of the two “measles” deaths, Aleph, wrote:
“… hospital care is deteriorating nationwide, not just in pediatrics. I expect death rates to rise and life expectancy to decrease.”
Care is ruled by convenience under the “least effort” principle. Hospitals are like a fragmented assembly line with the “product”, in fact a CLIENT, in one spot (a bed) and the workers moving along, each to do their “thing” but nothing else.
The two Texas girls’ deaths are examples of 1) preventable in-hospital mortality, 2) increased hospital-acquired infections, and 3) increased age-adjusted mortality rates (6 and 8-year-old generally healthy American girls should almost never die of a typical or even atypical infection in modern times). Further, as per this article by KFF:
“The country continues to have the highest rates of preventable hospitalizations, avoidable mortality, maternal and infant mortality, and chronic disease burden among high-income countries.”
The KFF report goes even further:
“Patient safety remains a concern, with medical errors contributing to significant morbidity and mortality. Low-quality care includes medication errors, diagnostic errors, and healthcare-associated infections that can adversely impact health outcomes.”
All of the above happened in the Texas measles cases. However, I refuse to believe that those cases were unique. Instead, I fear they result from disturbing trends impacting the healthcare workforce over the pandemic years.
I formulated ten dynamics within healthcare that I believe represent the “root causes” of the deteriorating quality of care.
I’d like to invite my readers to submit any additional thoughts on drivers of poor care quality beyond those I discuss below. Hang in and hold on, because I paint a pretty miserable picture of what is happening in Medicine. Disclaimer: I almost certainly “cherry-picked” data below to support my arguments, but that is OK I am happy to evaluate any contrary or contradicting data or opinions that have merit.
*Please consider a paid subscription if you appreciate the time and effort I put into performing these extensive case reviews and researching and writing my posts.
Hypotheses As To Why The Quality Of Medical Care In The U.S Is Deteriorating
1. Widespread Cognitive Impairment In the Wake of the Covid mRNA Campaign (and Covid)
It should be evident that physicians, nurses, and nurse practitioners were among this country’s most highly vaccinated subpopulations due to Biden’s Federal CMS mandates.
Just this week, a WSJ article highlighted the “millions of Americans,” both old and young, with new cognitive impairments due to “Long COVID” (which we know from what I bear witness to each day in my vaccine injury and Long COVID specialty practice—it is a euphemism for “Long Vax” – 70+% of my patients’ issues started in temporal association with vaccination, not COVID).
In addition, as per AMD, “the COVID vaccines were sold with the most aggressive marketing campaign in history, using healthcare workers as the initial cohort to promote the vaccines since it would be easy to;
1) manipulate them into fully vaccinating
2) have the public trust in their endorsement
3) make them less likely to publicize the side effects of the shots
Because of this, doctors and nurses were some of the most highly vaccinated Americans, and in turn had some of the highest rates of injury.
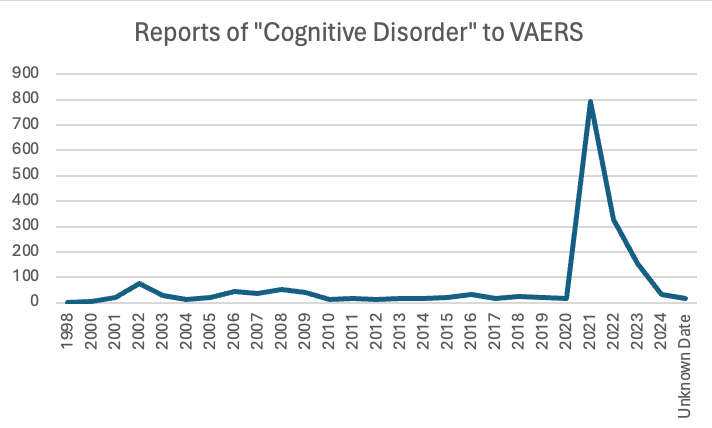
This is important because cognitive impairment is one of the most common side effects of the COVID vaccines, something not only shown by the data but also in my patients – neurological and cognitive injuries are the rule. The data supporting this reality is overwhelming:
- A recent study by Thorpe et al identified alarming increases in 86 adverse events related to brain function, behavior, and cognition following COVID-19 mRNA injection, and another study showed spike protein in the cerebral arteries of vaccinated individuals 17 months out.
- AMD’s compilation of data showing the negative cognitive impacts from the mRNA vaccines adds even more disturbing data on the vaccine’s impact on cognition.
- In a post I wrote about an interview I did with a veteran ER/ICU nurse at The Ohio State University Medical Center (TOSUMC), she reported that many of the illnesses and/or disabilities sufferred by physicians in that system were described to her as being due to neurological issues – either overt neurological deficits or cognitive decline/impairment, and even dementia.
- One study published in Nature (one of the top medical journals) reported that after mRNA vaccination, they found a 68% increase in depression, a 44% increase in anxiety, dissociative, stress-related, and somatoform disorders, a 93.4% increase in sleep disorders, a 77% decrease in schizophrenia, and a 32.8% decrease in bipolar disorder.
- Another study analyzed individuals over 65 and found Covid vaccination increased the risk of mild cognitive impairment by 138% and the risk of Alzheimer’s by 23%, with smaller increases in vascular dementia and Parkinson’s disease that the authors did not deem to be significant.
- VAERS detected a massive spike in cognitive issues being reported to it after the COVID-19 vaccines hit the market.
- Admissions to a nursing home significantly increased, as shown by this extensive data set from the Netherlands.
- Ed Dowd has repeatedly documented a significant increase in physical and cognitive disability throughout the adult population, beginning with the onset of the mRNA campaign:

- Steve Kirsch was contacted by a whistleblower who reported there had been a 25-fold increase in sudden dementia at the nursing home where she works.
- From Igor Chudov’s article on this topic:
I own a small business and deal with many people and other small businesses. Most provide reliable service, remember appointments, follow up on issues, and so on. I noticed that lately, some people have become less cognitively capable. They forget essential appointments, cannot concentrate, make crazy-stupid mistakes, and so on.
- Igor Chudov also identified another dataset from the Netherlands, which further corroborated a massive cognitive decline:
The latest quarterly research update from the GOR Network shows that in the first quarter of 2023, there was a 24% increase in GP [general practitioner] visits related to memory and concentration problems among adults (age 25 years and older) compared to the same period in 2020.
More specifically, they found:
•No increase was observed in adults under 25 years old.
•A 31% increase was observed in those 24-44.
•A 40% increase was observed in those 45-74 years old.
• An 18% increase was observed in those over 75 years old.
2. Workforce Shortages In The Wake Of The mRNA Campaign
- Numerous insurance company reports and studies of actuarial data on the vaccinated report a 37% lower life expectancy and a doubling of the risk of dying. Sun Life Financial’s US operations reported a surge in costly claims that caused stop-loss insurance benefits costs to spike in the fourth quarter.
- A new study found massive increases in deaths from Covid-19 in association with increased vaccination among Western Countries by up to 1,275.0%
- The Ethical Skeptic analysis of publicly available data finds that cancer diagnoses and expenditures began to skyrocket with the rollout of the mRNA campaign.
- The insane number of predominantly young, actively employed Canadian doctors whose deaths have been tracked on social media (132 at last count, two years ago).
- In my post on Ohio State University Medical Center, the nurse I interviewed reported that the new cancer center was running out of infusion suites and that cancer surgeries were being delayed due to the excess volume.
- Jeff Childers wrote a recent post on cancer clusters reported in numerous and diverse geographic regions, workplaces, and within families. Industrial exposures cannot be blamed given the diversity of cancers and the clustering of different cancers within the same family. The most alarming clusters are occurring among groups of nurses and/or doctors in the same hospital.
- More “real-world” evidence of the above comes from my interview with a veteran nurse colleague who has worked at OSUMC for decades. She reported:
- An increasingly noticeable number of doctors, nurses, and staff have “died suddenly,” “died unexpectedly,” or have become disabled and ill from injuries and/or cancer. The youth and health of these employees have been increasingly remarked on amongst staff (not to mention the deluge of previously healthy and/or young patients that are now presenting with severe and/or atypical (for that age) illnesses. Remember, cancer used to be a disease of aging essentially.
- The suspected role of the vaccines in most of the deaths is an open secret and a growing concern among staff there. Ohio State University Medical Center (OSUMC) stopped emailing out obituaries of prominent or veteran employees when they died. Why do you ask? Because of the uncomfortably noticeable large number of them, which triggered comments by employees openly calling out the likelihood that the vaccines were a cause (i.e., they would point out the dates of the deceased’s vaccination and their death). Unsurprisingly, she also told me that OSUMC would quickly censor any posts of that nature (despite containing no foul language, personal attacks, or threats). From a text conversation we had:
“Yes, this is huge. Lots of internal cases of death and disabilities. They quit posting internal obits for staff. The comments underneath them showed that people knew why everyone was dropping dead for baffling reasons. So those went away.”
- Several physicians (the most noticeable of them being super-specialists who cannot be easily replaced), besides dying, were also leaving due to disability or retiring due to unspecified health reasons.
- She heard of a growing number of lawsuits by family members of these physicians against OSUMC for the mandates that led to their deaths or disabilities.
- One lawsuit was filed by the widow of a physician who dropped dead suddenly. Interestingly, she demanded an autopsy with staining for spike protein, and the heart was found “loaded with spike.”
- When physicians die suddenly, this creates a huge mess operationally because “open notes” in the electronic medical record (EMR) can’t be closed, and the chronic, ongoing care of large numbers of often long-time or highly active patients becomes disrupted. In her words, “dealing with the practice of a doc who died is a mess – dealing with open notes, ongoing patient care, patient calls, and maintaining plans of care.”
- Many of the disabilities and deaths of physicians were discovered by this nurse while she was following up on notes that were “left open” in the EMR. The staff would then tell her about the injury, death, or disability of the health care provider who started the note. Further, adding the “abandoned” patient panel to healthier and still working physicians in that specialty was causing further strains.
- Cancers are exploding at OSUMC, causing massive strain on oncology services, particularly glioblastomas in the brain, as well as in the spine. Also, case managers for many cancer patients stated that they were not retiring due to the volume of patients in need.
- Even worse, cancers are being missed at high rates, given that the “index of suspicion” in younger patients is not appropriately high enough. As a result, doctors are missing cancers, as evidenced by retrospectively “obvious” signs and symptoms in the record.
- Applications for both short and long-term disability have risen so much that they have created backlogs and delays that staff have noticed and are more openly talking about. The often young ages of the staff applying for disability have not gone unnoticed either.
- She knows of several colleagues who are either declining or dying from cancer but are forcing themselves to work to provide for their families.
In a recent conversation with A Midwestern Doctor, they reminded me that we both know numerous doctors who have become impaired or disabled from the COVID vaccines, many of whom then had to enter early retirement, or sadly, died prematurely from a vaccine side effect. Many doctors are still in denial about this.
3. Physician, NP, and Nurse “Burnout” Rates Are Increasing
Physician “burnout” rates increased significantly during the COVID-19 pandemic, from 38.2% in 2020 to 62.8% in 2021. This spike marked an all-time high and ended a previous six-year decline in burnout rates.
In the articles I read about surging burnout rates, the above examples from OSUMC were evidenced by data findings (all references hyperlinked below).
- Increased Workload and Patient Volume: Physicians faced an overwhelming number of patients, especially during the COVID-19 surges
- Risk of Infection: Constant exposure to COVID-19 patients increased fear and anxiety about personal and family safety.
- Insufficient Resources: Early shortages of personal protective equipment (PPE), lack of effective treatments, and inadequate institutional support heightened stress.
- Staffing Shortages: Many healthcare systems experienced severe staffing shortages, which led to longer hours and more intense work for the remaining staff.
- Work-Life Imbalance: School closures, increased childcare demands, and inability to maintain work-life boundaries contributed to distress.
- Emotional and Psychological Strain: Physicians reported increased anxiety, depression, insomnia, and a sense of helplessness in the face of high mortality and suffering.
- Moral Distress and Mistreatment: Experiences of mistreatment by patients or the public and politicizing public health measures compounded stress.
- Administrative Burdens: Ongoing frustrations with bureaucracy, documentation, and loss of autonomy further eroded professional fulfillment.
These factors combined to create an unprecedented level of occupational distress among physicians during the pandemic, with many considering leaving the profession or reducing their clinical hours.
This is probably a good time to mention that, although I was shocked by the inept medical care in the two non-measles deaths, the above may provide some forgiving context for their actions. Providers are now up against many adverse dynamics while caring for patients, so some grace must be shown. I prefer to think of the doctors as “doing the best they could,” against the many stresses preventing them from delivering the quality of care patients expect and deserve.
4. Attrition Of Physicians From The Workforce
The implications of the rising cognitive issues, deaths, and burnout are that they are leading to an increased physician attrition rate in the United States. Lo and behold:
- Job Changes and Retirement: A 2022 survey found that 43% of physicians changed jobs during the pandemic, 8% retired, and 3% left medicine for non-clinical careers—much higher than typical annual turnover rates of 6–7%.
- Annual Attrition Trends: Before the pandemic, annual physician turnover increased from 5.3% in 2010 to 7.6% in 2018—a 43% increase. In 2022, 40% of U.S. physicians reported an intention to leave their current job within the next two years. This figure decreased slightly to just over a third (approximately 33–35%) in 2023 but is still historically high.
- Specialty and Demographic Variation: The increase in attrition has not been uniform across all specialties or demographics. For example, primary care and rural practice have seen sharp declines in new entrants, and older physicians (65+) are retiring at higher rates.
Now, although attrition has risen, the overall physician workforce has grown. However, that is almost certainly being driven by recruiting less experienced, younger, and/or international doctors with varied training. Most physicians who leave the field do so for retirement between the ages of 60 and 69. Thus, the older, wiser, veteran doctors are leaving at unprecedented rates. If the most knowledgeable and experienced docs are leaving, who is going to “teach” what used to be called “the art of medicine?”
5. Attrition of Nurses From The Workforce
If you thought the rising attrition rates of doctors were bad, it gets way worse with the nurses. Since the onset of COVID-19, the annual nurse attrition (turnover) rate in the U.S. has also increased significantly. The numbers are eye-popping – multiple studies and workforce reports have documented a sharp rise in both departures and nurses’ intentions to leave the profession.
- During the pandemic, about 100,000 registered nurses left the workforce in two years, primarily due to stress, burnout, and retirement.
- The psychological impact of the pandemic included increased workload, exposure to critical illness and death, and emotional exhaustion.
- **Projections indicate the situation may worsen: If current trends continue, nearly 900,000 RNs (about one-fifth of the U.S. nursing workforce) are expected to leave the profession by 2027.
One-fifth of the U.S. nursing workforce is expected to leave the profession in the next two years? We have to stay out of the hospitals, folks.
6. Increases in “Sentinel Events” Within Hospitals
Based on the above data showing that healthcare providers likely suffered some of the highest rates of cognitive impairment, neurological conditions, cancers, and sudden deaths, which then caused skyrocketing burnout and massive workforce departures, it should come as no surprise that there is a disturbing data trend regarding “sentinel events” in hospitals. First, let’s go over the definition of a sentinel event:
A “sentinel event” is an unexpected occurrence in a healthcare setting that results in:
- Death
- Permanent harm (e.g., loss of limb or function)
- Severe temporary harm (e.g., significant disability or disfigurement)
These events are unrelated to the natural course of the patient’s illness and are often caused by major mistakes or negligence by healthcare providers. Sentinel events are closely investigated by healthcare regulatory authorities to identify root causes and implement corrective actions to prevent similar incidents from occurring in the future.
There are 58 total types of sentinel events, with the most prevalent being:
- Falls (48%)
- Wrong site surgery (8%)
- Unintended retention of foreign object (8%)
- Assault/rape/sexual assault/homicide (8%)
- Delay in treatment (6%)
- Suicide (5%)
Check out the data chart below from the Joint Commission’s 2023 review of sentinel events, which shows a steep rise in sentinel events concurrent with the rollout of the mRNA platform (obviously, other factors likely contribute, but the temporal association should give serious pause):

So, what sentinel events drove this rapid rise?
Answer: FALLS!

The average number of falls in 2019 and 2020 nearly tripled in 2021 and then quadrupled the pre-pandemic rate in 2022 and 2023. Admittedly, this can be due to the increasing cognitive impairment of patients, but it also likely represents less monitoring/care/training of nurses (issues discussed in my previous post here). But the real shock is how the Joint Commission addressed this issue in their report:
Conclusion: Reported sentinel events remained consistent with previous reporting patterns. Consistent with prior years, patient falls were the leading event type reviewed (48%).
I no longer am shocked by “authorities” so blatantly and willfully peddling lies, misrepresentations, and distortions. But this takes the cake. Yes, the highest percentage of sentinel events were falls in “previous years.” However, if you look below to see what percent were falls before the jab campaign, only 18-21%. They are almost 50%, and the absolute number of falls reported has skyrocketed. “Consistent with previous years” my ass.

From the Joint Commission Report:

26 deaths from falling in a hospital? Fifty-six falls resulted in permanent harm? Five hundred thirty-eight resulted in severe harm?
Why is there not a big national push to prevent hospital falls if they have suddenly risen at such an acute and unprecedented rate? This metric screams that hospitals are now much more dangerous places, given that they cannot prevent falls among the patients they care for. Again from the report:
Consistent with 2022, patient falls while ambulating was the leading mechanism for falling, followed by falling from bed and while toileting. Reported contributors to falls included policies not being followed (e.g., fall risk assessment), lack of competency to recognize abnormal clinical signs or signals, inadequate staff-to-staff communication during handoffs or transitions of care, and lack of shared understanding or mental model regarding plan of care.
7. Impacts of Diversity, Equity, and Inclusion Policies
The text exchange below is with a former close colleague (one of the few still inside “the system” I still communicate with). His opening statement below was his response to reading my study on the variation in performance of ICU docs. He lamented that he was doing less “ultrasound” of patients’ lungs on daily rounds (a practice I had taught him and which I religiously followed during my daily ICU rounds):
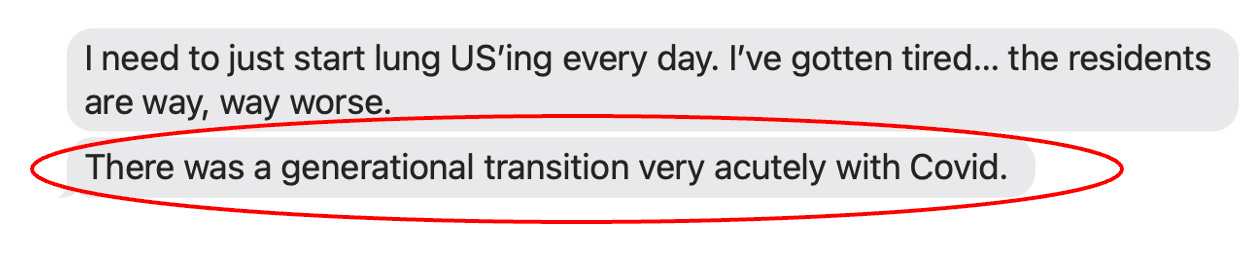
I asked him to “say more” (oddly, I was already drafting this post at the moment of this exchange last week, and what he was about to write was not on my radar (yet):
His comment about “unit (ICU) weeks becoming even more exhausting than baseline” triggered pain in me. Know that ICU specialists in major academic medical centers typically work one ICU week a month (the rest of the time, I captained other inpatient pulmonary services, bronchoscopy suites, outpatient practice, or I was doing research, administration, and teaching).
“ICU weeks” began on a Monday morning and ended on a Monday morning. As one was approaching, you began to feel a bit of dread/anxiety, and as one finished, it typically took a few days until you felt “normal” again, or at least somewhat rested and relaxed. It was repeatedly disruptive to the ever-elusive “work-life balance” we all seek.
And that is because ICU weeks were intellectually taxing (on an average day I made about 700 clinical decisions, an overstatement but you get it), emotionally draining (10- 20% of my patients died within insane family dynamics driven by loved ones unable to accept the reality of death), and physically depleting (due to seeing so many complex patients combined with often little or interrupted sleep). Based on what my colleague said above, I can’t imagine what they are like now—another reason to show grace to the ICU doctors caring for Daisy and Kaley.
One of the most alarming insights in the text exchange above was his comment that the system is now viewed more overtly as a profit-driven machine, stifling those who might otherwise be inspired to lead impactful improvements in care delivery or therapeutics.
That comment saddened me because, in my career, I was always studying, experimenting, and trying to improve care and outcomes using promising therapies or novel diagnostic devices. That goal inspired my work and my teaching, which similarly inspired my trainees, always to be thinking and reflecting on approaches that could be more impactful. That quality led to my career achievements and garnered me respect and accolades. To hear that doctors now are not similarly inspired, nor is it possible for them to “innovate” due to entrenched economic interests and/or rigid protocols, is truly damning for the future.
The two reader comments below encapsulate the consequences of what I discussed above:
As senior veteran pilot Sherry Walker testified to Tucker Carlson concerning the causes of all these flight mishaps, I would like to know if the medical establishment is also downgraded to inexperienced young know-it-alls and DEI-forced medical school applicants, and this is where we The jab-induced cognitive and neurological impairments that negate sound judgment could also come into play. Or is this stuff intentional, like the forced vents and Fraudci drug protocol?
My daughter is a surgical oncologist for head and neck. She was trained at top hospitals. She’s seen some things about hospital care these days that trouble her, and she’s been criticized for pointing out areas that need improvement. Her boss pointed out that the place she works is unlike the top ENT residency hospital where she was trained. Unfortunately, this increases my pessimistic view of health care. So I’m not surprised at what happened here, but to lose a child is devastating. What is tragic is that money is now more important than people.
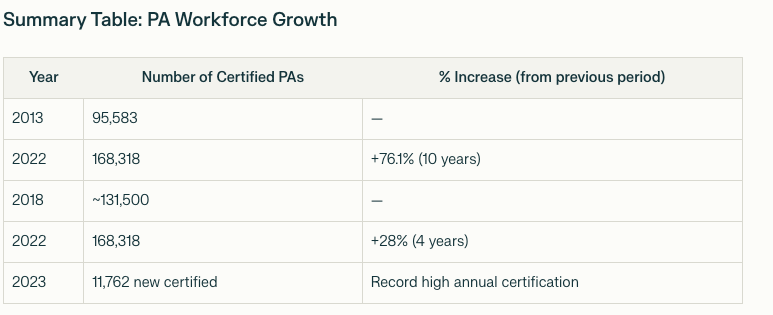
8. The Proliferation Of Lower-Cost, Less Experienced Nurse Practitioners and Physician Assistants
This is a sensitive issue because, in my practice, I primarily work with nurse practitioners (NPs). My partner, Scott Marsland, is an NP who is one of the best clinicians I have worked with in my career. The other NP’s on my team are equally impressive because 1) we were very careful in our selection of them, 2) they are veteran nurses with tons of experience in nursing while also having years of NP experience which have led them to being highly skilled and empathetic clinicians and 3) we developed a practice of “letting someone go” quickly if we felt they did not “have it.” We did that on numerous occasions. As a result, the NP’s at our Leading Edge Clinic are top notch.
The problem is that things have changed in the NP world. Now, many aspiring nurses go to nursing school and then go straight into NP training or do so after short, limited bedside nursing experiences.
Recent discussions and anecdotal evidence from practicing NPs and educators highlight that it is increasingly common for individuals to become NPs with as little as two to three years of RN experience, or sometimes even less, due to the expansion of direct-entry and accelerated NP programs. They do this not only because of the better compensation of NPs but also because hospitals have a great interest in expanding the pool of NPs, given that their labor costs are far lower. To wit:
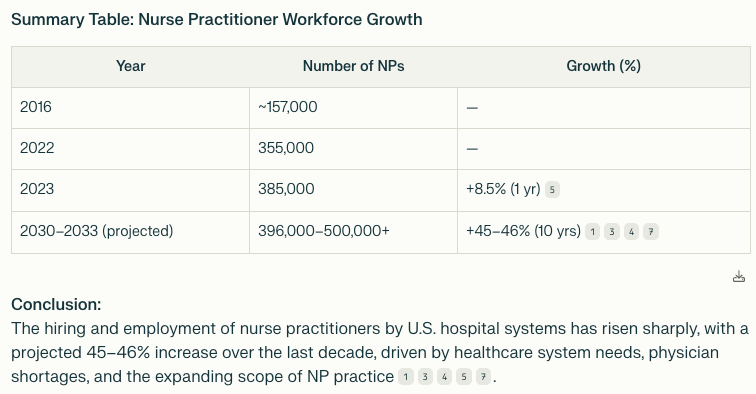
And it is only going to get worse. According to the U.S. Bureau of Labor Statistics, nurse practitioner jobs are projected to increase by approximately 45–46% over the decade from 2023 to 2033, making it the fastest-growing occupation in the country.
What about physician assistants? The U.S. Bureau of Labor Statistics projects that PA employment will grow 27–28% from 2022/2023 to 2032/2033, which is much faster than the average for all occupations.
If you think the above is bad, it gets even worse. Again, from a comment by one of my subscribers named Aleph:
“Here in California, someone who works at Kaiser told me they already use AI for some services but were told to keep it secret.
I don’t doubt that PROFIT is a primary decision factor in their AI.
My mother needed physical therapy; they outsourced it to an “agency.” A “therapist” was sent, but from previous experience, I noticed something was off, like missing an initial assessment of the patient’s condition. The “therapist” didn’t even know what my mother’s condition was, but started her “work”. Long story short, I found out she was not even a licensed Physical Therapist, but just an assistant, and she did not even know the name of the therapist in charge..
Note of color, a friend of mine needed Speech Therapy. The “speech therapist” tried to communicate and set an appointment through TEXT MESSAGES… let that sink in!
I worry about another downstream effect of having more and more NPs responsible for direct patient care: I fear it may “dilute” doctors’ clinical experiences and skills due to their having to see fewer patients directly. Although NP’s are indeed, early on, directly “overseen” by physicians, I argue that oversight responsibility does not fully translate into the physicians’ direct clinical experience of constantly evaluating and shifting assessments and treatments accordingly.
My point is that the primary skill that makes an “expert physician” is “pattern recognition.” To acquire deep powers of pattern recognition, you need to see thousands of patients, up close, personally, with direct responsibility, daily engagement, and focus. A doctor who has 3,000 patient care experiences versus one with only 500, and you are talking about two different doctors. Similar to a piano player with 10,000 hours of practice under their belt versus one with 2,000. They can’t play the same tunes, nor with the same beauty or skill.
I recall reflecting on my career development at one point, when I realized how long it took me before I had started to “feel like an expert.” I pinpointed that transition to almost three years after becoming an “attending” physician (e.g., after finishing four years of medical school, three years of residency, three years of subspecialty fellowship training, and then three years as an attending).
My first days out of fellowship as a young attending physician were frightening. Being in complete charge of an ICU team without direct oversight caused daily anxiety because I still had a lot of uncertainty (lack of confidence) about my diagnoses and treatment decisions. I was very cerebral and arithmetic in my approach, relying on analyses of masses of disparate data that often conflicted and/or were shifting rapidly. I was not an expert, but I was “in charge” and doing my best with what I had.
Then, a few years later, as I walked into a new patient’s room on rounds with my trainees and I looked at the patient while listening to the case history given by one of the fellows. I suddenly realized I knew exactly what was wrong with him with little information. I just knew. When all the subsequent data supported my initial suspicion, I recall that being an impactful moment. It was a confusing case, and my suspicion turned out to be spot on. I remember thinking, “How did I know that?”
Simple – whatever was wrong with that man, it was in a pattern I had seen in patients with the same diagnosis. That experience then kept happening more and more. I noticed I would intuitively focus on and identify key aspects of a patient while automatically ignoring what would later turn out to be unimportant. I began to do this almost subconsciously, rather than by amassing all the data and then deliberately sifting through all possibilities and probabilities. It switched from the cerebral to the intuitive. My work became much easier afterward; I was also much quicker, more accurate, and more effective. But it took years!
One caveat that is relevant to this argument: in my first two years as an attending, I worked in a chronically short-staffed Pulmonary and Critical Care Division (with no NPs), so I was billing 250% of the amount an average ICU doctor bills in one year. My hospital was worried at one point that they would be investigated for fraud.
But there was no fraud. I was forced to see an obscene number of patients and worked like an absolute madman to do so. I commuted by train and would obsessively read up on my patients’ issues. But it was like a trial by fire—I came out the other side with deep powers of intuition and experience. I wonder if that would happen today if I relied on NPs to see many of the patients or do most of the clinical interactions.
9. Expansion Of Standardized Treatment Protocols At The Expense Of Critical Thinking Skills
Before Covid and my excommunication from the medical system, I loved my career – I was an “intensivist” running ICUs, challenged by the “sickest of the sick,” which required me to find new therapies or approaches when traditional treatments were failing. I was a pioneer in developing and employing specific innovations in my specialty which led me to national and sometimes international acclaim – specifically with the use of therapeutic hypothermia for cardiac arrest, physician performed bedside ultrasonography for rapid identification of organ failure states, and the use of IV vitamin C, thiamine and corticosteroids in sepsis (the Marik protocol).
Beyond that, if someone was in a complete cardiovascular collapse, I could call for emergent infusions of methylene blue, I could use high-dose steroids, I could use Marik’s protocol in non-sepsis conditions, I could use thrombolytics empirically in emergencies, etc.. I did the best I could with often obscured, incomplete, and shifting information as to the actual driver of illness in a crashing patient. I did things without massive randomized controlled trials to support my approach. I could be a “cowboy” when a clinical situation demanded it.
What started to worry me in COVID is that Paul and I would get consulted by family members of severely ill COVID-19 patients who were in a hospital (until we started refusing them due to futility). Over and over we observed cases where the doctors would not “change what they were doing” – they would not try empiric higher dose steroids, not try blood thinners in states of clear hypercoagulability, not add high dose ivermectin in failing cases, not try high-dose IV Vitamin C, not try fluvoxamine or anti-androgen therapy (all beneficial in Covid).
I was shocked that they were sticking to the same lame protocol of low-dose dexamethasone, remdesivir, etc in the face of a deteriorating patient. I could not believe our nation’s doctors had stopped doctoring and were instead cowed into submission. It was clear that they were being restricted by heads of hospital committees, pharmacists, and bureaucrats who kept calling for “standardization of treatment approaches” – brazenly oblivious that illnesses and patients are not standardized, as they tend to be more often unique than similar.
I also hypothesize that the weaponized medical boards, societies, and agencies that persecuted outpatient COVID-19 doctors for trying off-label treatments have similarly impacted the psyche of hospital doctors, creating renewed reluctance to treat someone “off-label” or “without sufficient evidence.” I have to admit, though, that the one “bright spot” in the two “measles deaths” is when the doctors decided to treat Daisy with IVIG based on a solid rationale but minimal clinical evidence. So, the spirit for that kind of doctoring still lives, but is becoming rarer, I fear.
10. Corruption And Distortion Of “Evidence-Based Medicine” and The Religious Adherence To Randomized Controlled Trial Data.
Early in Covid, I, along with several close colleagues of mine working at Northwell on Long Island (I had trained with nearly all of the interviewees in the article), were profiled in the below NYT Magazine article:

Like the rest of society, which became deeply polarized due to relentless propaganda, doctors have been propagandized with conflicting notions of “evidence-based medicine” (EBM). Few are aware that the earliest iterations of EBM principles did not say to only rely on RCT data to guide treatment; the original principle was, as per David L Sackett’s widely cited article from 1996, defined as “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients.”
Put differently, Sackett, proposed that three different considerations needed to be weighted equally in evidence based clinical practice:
•Patient Values
•Clinical Expertise
•Relevant Research
In the above article about the various approaches doctors took to treating a novel disease, the journalist described the two camps of doctors in Covid. The first were those that felt using unproven treatments for a novel disease was “experimenting and unethical” and thus, 1) “supportive care only” approaches should be the mainstay and 2) any “unproven” treatments should only be studied in the context of a clinical trial. The other camp felt that any treatment with a strong clinical and/or mechanistic rationale and tolerable safety record was “reasonable to try.” I am certain my readers know which camp I was in :).
First, it was obvious that “supportive care only” was failing from the first patient I saw. They were visibly clotting dialysis circuits, their lungs were severely inflamed in an organizing pneumonia pattern (a condition which is treated with corticosteroids), and most notably, their lungs were uniquely “dry.” Yet, my superiors were advocating for supportive care only, and then my Chair of Medicine influenced my fellow Covid therapeutic committee members to remove IV vitamin C from the University protocol, despite the fact that I had provided sufficient evidence for including it in the treatment of severe lung injury.
I viewed this as scientific misconduct, which triggered my final decision to resign (something I had been contemplating for weeks). I refused to serve as a leader if I was being forced to sacrifice my judgemen, expertise, and morals for some perverse notion of EBM.
Here is one quote from the article that is pretty telling in terms of how heated it got within hospitals, taken from what I call an “evidence-based maniac”:
Spyropoulos recalls that he talked to the group of front-line doctors about the importance of high-quality, randomized trials in making scientific progress and the risks of trying experimental treatments without them. “I stressed to the group that we should not abandon this principle, even in the very stressful environment of a pandemic that was overwhelming our hospitals at Northwell,” he said. Relying on gut instinct rather than evidence, he told them, was essentially “witchcraft.”
So I am a witch now? At the risk of seeming immature or petty, this is the photo of that guy included in the article. Who is the witch, sir?

But let’s be clear, this guy literally argued that we need to prioritize the principle of conducting RCT’s to further scientific progress… over making the care of the patient our primary consideration. I guess I missed that course in medical school which prioritizes the conduct of research over the welfare of the patient. My God.
Know that the opposing viewpoint quoted below was from Dr. Mangala Narasimhan, a very close colleague of mine (she was my senior fellow when I was in training, and I taught ultrasound with her across the country for years):
Dr. Narasimhan knew researchers were concerned that in prescribing tocilizumab so readily, physicians were possibly hampering enrollment in the trial underway at her hospital for sarilumab — a patient who received tocilizumab could not also receive sarilumab. She and her team did not prioritize the trials; they wanted to provide the drugs they thought were needed. “We’ve always been allowed to choose treatment, right or wrong, based on what we thought was best,” Narasimhan said in May. “And that was gone. It was hard.”
A quote from another physician:
In April, he learned that Massachusetts General Hospital was starting a randomized, controlled trial for tocilizumab. “If that were my loved one,” he said, imagining a family member who might receive a placebo in that trial, “I’d be upset. I’d think, Why am I doing this? If it’s an off-label use with an approved drug — give the damn drug to everybody.”
The journalist then concluded the section with:
In addition to fighting resistance from their administrators, the doctors were sometimes also at odds with their colleagues, especially infectious-disease doctors, many of whom believed that anti-inflammatories like tocilizumab and steroids could do more harm than good. “You’re killing these patients,” one infectious-disease doctor told Hahn at Long Island Jewish.
At the risk of making this post too long (you still with me?), I decided to include the sections of the article focused on my early Covid battles with “the system” because it best illustrates my stance on the issues raised above.
Pierre Kory, the Wisconsin critical-care doctor, sees a different medical lesson emerging from the pandemic: that the emphasis on randomized, controlled trials can get in the way of doctors’ providing common-sense, lifesaving treatments.
In April, supportive care alone was considered the best option for patients with Covid-19, given that there was no evidence yet to back other treatments. Kory, who was then the chief of critical-care service at the University of Wisconsin Hospital and Clinics, believed instead that medications commonly used in critical care would most likely help critically ill Covid-19 patients, too. That month, at a well-attended meeting with fellows, residents and leadership, including Lynn Schnapp, the chair of the department of medicine at the University of Wisconsin medical school, Kory suggested an approach that went beyond supportive care. He had been consulting with senior hematologists at the hospital and had observed alarming blood clotting in Covid-19 patients. He and the hematologists proposed that the hospital consider administering an aggressive dose of anticoagulants to patients whose blood tests showed elevated risks for clotting. (Many medical-society guidelines that once called for only supportive care now recommend the use of anticoagulants in Covid-19 patients, but not in doses as aggressive as those that Kory and specialists at the hospital had proposed.) (Ed: as variants changed, so did their clotting dynamics – I myself became less aggressive as time went on, something I like to call “doctoring”).
The meeting among Kory and his colleagues took an adversarial turn. “No one else is doing this,” said Lynn Schnapp, as Kory recalls. (She denies saying that, although a former colleague of Kory’s who attended the meeting confirmed Kory’s account.) “There is no evidence,” a fellow I.C.U. doctor said more than once, her voice raised. Kory, who pointed out at the meeting that his suggestion was based on the opinion of the hospital’s own experts, says he fired back with equal intensity. “And this is Wisconsin,” he told me. “People don’t yell here.” Other colleagues who were supposed to jump off the call to attend another meeting later confided to Kory that they couldn’t bring themselves to leave, for fear of missing out on this unusual hospital drama.
At a subsequent, smaller meeting, Kory brought up with Nizar Jarjour, a division chief, the possibility of giving steroids, commonly used on critical-care patients, to Covid-19 patients in the I.C.U. “I don’t want to talk about it,” Jarjour said.
In a lengthy email Jarjour later sent me, he explained that open discussion was welcome during that period of time; he also sympathized with the sentiments of the I.C.U. colleague who was urging caution while facing a novel virus.
Corticosteroids have a complicated and controversial history in critical-care medicine. Numerous trials over the past 50 years have been conducted on their efficacy in patients with acute respiratory distress syndrome, or ARDS, a diagnosis for patients who have reached a stage of perilous respiratory failure. Because many of those patients at that stage of illness have confounding factors, findings are far from definitive. But based largely on some meta-analyses, including those looking at how patients with MERS and SARS fared, the World Health Organization advised, early in the pandemic in this country, against the use of steroids in Covid-19 patients experiencing ARDS, which is to say, most patients on ventilators.
Kory and several colleagues at hospitals around the country noted that the studies that the W.H.O. cited, for example, were largely not randomized and controlled; other relevant institutions like the Society of Critical Care Medicine, whose doctors treat the most ill patients, and the European Society of Intensive Care Medicine did recommend the use of steroids for ventilated Covid-19 patients with ARDS. Also, in Kory’s own clinical experience, corticosteroids could be lifesavers. He did not see them as a wild-card drug for this disease, like hydroxychloroquine; he used them for non-Covid-19 patients who were facing cytokine storms or ARDS. He was surprised by the heat with which colleagues challenged him when he made the recommendation, and he believed that his own leadership role in conference calls subsequently diminished. He and Jarjour, he said, had more disagreements in three days than they had in the previous five years.
On April 7, Kory’s colleague Ellie Golestanian sent an email to Kory and others, at 1:32 a.m., in response to another colleague’s call for the use of corticosteroids and anticoagulants: “In patients with severe Covid-19, we are fumbling in the dark, clutching at anything that might work. But as you are well aware, just because a therapy ‘should’ work, or we desperately ‘want’ it to work — it does not follow that it ‘will’ work.”
“When I hear stuff like corticosteroids described as experimental and unproven, I want to jump out a window,” Kory told me later that month. “They make it sound like we are experimenting on people. I want to be respectful of my colleagues, but I feel like they are getting it 100 percent wrong. I’ve never seen smarter people get a problem more wrong. Because they are running hypotheses in a lab and so many of them fail, they think when I approach a patient, I am testing out a hypothesis. It’s not like a hypothesis, but more like a problem, and I have to figure out how to fix it with a couple of decades of experience to back me up. It’s a stretch to call it a hypothesis. It’s just me doctoring.”
Kory was so frustrated about the hospital’s approach that in May he resigned, taking a job instead at Aurora St. Luke’s Medical Center in Milwaukee. “Our differences were so far apart, I felt I couldn’t be a part of it,” said Kory, who foresaw, in April, a “catastrophe” if doctors at any hospital could apply only supportive care. A colleague of his in New York, an I.C.U. doctor affiliated with a major medical center, confirmed that he, too, resigned from his hospital, in part because of tensions around his decision to try an F.D.A.-approved medication off-label and outside a trial. In May, Kory, following his disagreement in Wisconsin, spent several weeks in New York treating patients, often with steroids.
In June, Oxford posted a preliminary report for its Recovery trial of more than 6,000 patients who received either standard care or dexamethasone, a steroid similar to the ones that Kory and other I.C.U. doctors had been advocating. At least when administered to patients who were already on oxygen or ventilators, the drug saved lives.
Kory sees, in the Oxford results, a story of triumph. He believes that he successfully treated patients with steroids and that the Recovery trial results prove it. And yet if patients did not respond, he would go further, increasing the dose, in a few instances, to a level 10 times as strong as that in the trial. Did the higher dosage increase the risk? A research purist like Kevin Tracey would point out the answer to that question is still unknown. Despite the enthusiasm for the Recovery trial, Tracey maintains that even one stellar randomized, controlled trial does not settle the question of the use of steroids for patients with COVID-19. “It needs to be replicated,” he said. Given the long, complicated history of steroid studies, he predicts that sometime down the road another statistically powerful randomized, controlled trial will yield contradictory findings. In Tracey’s reservations, Kory sees not rational evaluation but bias. “That’s a 6,000-person trial he’s discrediting,” Kory said. “That’s a person who will never be convinced.”
Kory is also part of a group of critical-care doctors who widely disseminated a protocol for treating COVID-19 that includes anticoagulants and steroids but also other treatments—including Pepcid and intravenous vitamin C—whose efficacy is hotly contested among doctors.
Should Kory and his colleagues have been administering steroids when they did? Were they right? Kory thinks so. But Eric Rubin, the editor of The New England Journal of Medicine, thinks it’s not so clear-cut. “You could also say he was lucky,” Rubin said. (Ed: This quote is how I earned the nickname “Lucky Pierre” from Paul Marik 🙂
At times, throughout several conversations, Rubin defended the bond between doctors and patients, the need for physician autonomy, the necessity of making judgments in the absence of evidence, especially when mortality rates were so high; at other times he seemed frustrated that doctors were still relying on treatments for which there was no evidence, concerned that a lack of equipoise had possibly muddled the course of research. “I know I seem to be saying opposite things,” he admitted. “And I agree with myself.
Ultimately, the appetite for doctors to “try new treatments” in the political and scientific context of Covid was severely dampened by all the above and I believe continues apace. Thus, my concern is that this new, hardened paradigm will shift to illnesses beyond Covid – causing even less doctors to “try new things” for fear of “getting into trouble” or worse “having pharmacy refuse to provide the treatment” because it is not “FDA approved” or not sufficiently “evidence based.” Their ability and desire to innovate or even to take calculated risks on behalf of their patients will further worsen outcomes and care as we go forward.
Conclusion
Ultimately, the pandemic underscored that evidence-based medicine was never meant to be a rigid hierarchy, but rather a dynamic process that integrates the best available evidence (while continuously integrating evolving/emerging data), clinical expertise, and patient needs, especially amid unprecedented uncertainty. That reality is ever present, but is ever more difficult to navigate due to widespread injuries and deaths of health-care providers, massive attrition rates due to burnout, stifling of innovation, and replacement with less experienced, lower-cost providers. If this continues, which I have no reason to suspect it won’t, I see much more misery ahead, which is why a primary focus of my readers should be.. staying out of hospitals to any extent possible.