There was a doctor in Texas that conducted a near death experience experiment at his hospital after seeing a presentation on it at his church which he thought at the time was hogwash. They developed a questionnaire at his hospital that asked certain questions about the experiences as doctors encountered them including resuscitation efforts, which kept doctor bias out of the information gathering. Because of the way patients are draped for some surgical procedures they couldn’t see what was happening with their resuscitation efforts when they died, but a few cases explained being out of their bodies and seeing them trying to revive them, going to heaven to meet beings of light radiating love, some meeting Jesus, some meeting dead loved ones, undergoing life reviews, with others having much darker experiences before being sent back. But the common thread was all led changed lives after the experience, and those few cases proved their out of body experience was legitimate or they wouldn’t have been able to explain the resuscitation efforts witnessed. The take away is that the spirit lives after the chemical machine dies, and life after death is something to take very seriously with eternal consequences. So enter in a new study with some interesting results.
https://nyulangone.org/news/patients-recall-death-experiences-after-cardiac-arrest
Up to an hour after their hearts had stopped, some patients revived by cardiopulmonary resuscitation (CPR) had clear memories afterward of experiencing death and while unconscious had brain patterns linked to thought and memory.
This is the finding of a study led by researchers at NYU Grossman School of Medicine, in cooperation with 25 mostly U.S. and British hospitals, in which some survivors of cardiac arrest described lucid death experiences that occurred while they were seemingly unconscious. Despite immediate treatment, less than 10 percent of the 567 patients studied, who received CPR in the hospital, recovered sufficiently to be discharged. However, 4 in 10 of those that survived recalled some degree of consciousness during CPR not captured by standard measures.
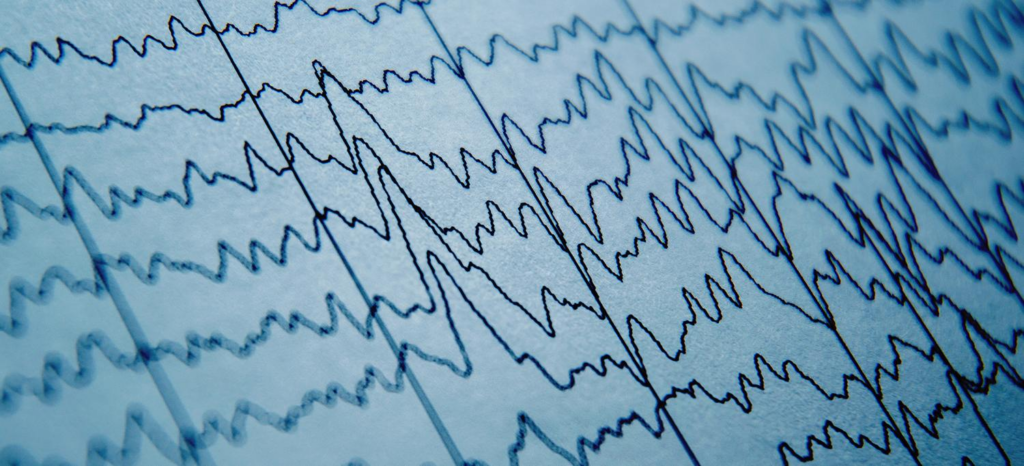
Published online September 14 in the journal Resuscitation, the study also found that in these patients, nearly 40 percent had brain activity that returned to normal, or nearly normal, at points even an hour into CPR. As captured by electroencephalogram (EEG), a technology that records brain activity with electrodes, the patients had spikes in the gamma, delta, theta, alpha, and beta waves associated with higher mental function.
Survivors have long reported having heightened awareness and powerful, lucid experiences, say the study authors. These have included a perception of separation from the body, observing events without pain or distress, and a meaningful evaluation of their actions and relationships. The new work found these experiences of death to be different from hallucinations, delusions, illusions, dreams, or CPR-induced consciousness.
The study authors hypothesize that the “flatlined,” dying brain removes natural inhibitory (braking) systems. These processes, known collectively as disinhibition, may open access to “new dimensions of reality,” they say, including lucid recall of all stored memories from early childhood to death, evaluated from the perspective of morality. While no one knows the evolutionary purpose of this phenomenon, it “opens the door to a systematic exploration of what happens when a person dies.”
“Although doctors have long thought that the brain suffers permanent damage about 10 minutes after the heart stops supplying it with oxygen, our work found that the brain can show signs of electrical recovery long into ongoing CPR,” said senior study author Sam Parnia, MD, PhD, an associate professor in the Department of Medicine at NYU Langone Health. “This is the first large study to show that these recollections and brain wave changes may be signs of universal, shared elements of so called near-death experiences.”
These experiences provide a glimpse into a real, yet little-understood dimension of human consciousness that becomes uncovered with death, adds Dr. Parnia, who is also director of critical care and resuscitation research at NYU Langone. The findings “may also guide the design of new ways to restart the heart or prevent brain injuries, and hold implications for transplantation.”
Called the AWAreness during REsuscitation (AWARE)-II study, it followed 567 men and women who experienced cardiac arrest during hospital stays between May 2017 and March 2020 in the United States and United Kingdom. Of the 567 patients, only 85 were monitored via EEG to measure brain waves during their experiences. The researchers first presented the study findings at a resuscitation science symposium, part of the American Heart Association’s Scientific Sessions 2022 in Chicago on November 6.
Only hospitalized patients were enrolled to standardize the CPR and resuscitation methods used, as well as recording methods for brain activity. Additional testimony from 126 community survivors of cardiac arrest with self-reported memories were also examined to provide greater understanding of the themes related to the recalled experience of death.
The study authors conclude that research to date has neither proved nor disproved the reality or meaning of patients’ experiences and claims of awareness in relation to death. They say the recalled experience surrounding death merits further empirical investigation, and plan to conduct studies that more precisely define biomarkers of clinical consciousness and that monitor the long-term psychological effects of resuscitation after cardiac arrest.
Funding and support for the study was provided by NYU Langone, The John Templeton Foundation, and the Resuscitation Council (UK) and National Institutes for Health Research in the United Kingdom.
Along with Dr. Parnia, other NYU Langone study investigators were Tara Keshavarz Shirazi, BA; Caitlin O’Neill, MPH; Emma Roellke, MD; Amanda Mengotta, MD; Thaddeus Tarpey, PhD; Elise Huppert, MD; Ian Jaffe, BS; Anelly Gonzales, MS; Jing Xu, MS; and Emmeline Koopman, MS. Other study investigators are Deepak R. Pradhan, MD, at NYC Health + Hospitals/Bellevue in New York City; Jignesh Patel, MD, Linh Tran, MD, Niraj Sinha, MD, and Rebecca Spiegel, MD, at Stony Brook University; Shannon Findlay, MD, at the University of Iowa; Michael McBrine, MD, at Tufts University; Gavin Perkins, MD, at the University of Warwick in Coventry, UK; Alain Vuylsteke, MD, at Royal Papworth Hospital National Health Service (NHS) Foundation Trust in Cambridge, UK; Benjamin Bloom, MD, at Barts Health NHS Trust in London, UK; Heather Jarman, RN, at St. George’s University Hospitals NHS Foundation Trust in London; Hiu Nam Tong, MD, at Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust in King’s Lynn, UK; Louisa Chan, MD, at Hampshire Hospitals NHS Foundation Trust in Hampshire, UK; Michael Lyacker, MD, at Ohio State University; Matthew Thomas, MD, at University Hospitals Bristol and Wexton NHS Foundation Trust in Bristol, UK; Veselin Velchev, MD, at St. Anna University in Sofia, Bulgaria; Charles Cairns, MD, at Drexel University; Rahul Sharma, MD, at Weill Cornell Medicine; Erik Kulstad, MD, at the University of Texas Southwestern; Elizabeth Scherer, MD, at the University of Texas San Antonio; Terence O’Keeffe, MD, at Augusta University; Mahtab Foroozesh, MD, at Virginia Tech; Olumayowa Abe, MD, at NewYork-Presbyterian; Chinwe Ogedegbe, MD, at Hackensack University; Amira Girgis, MD, at Kingston Hospital NHS Foundation Trust in Surrey, UK; and Charles Deakin, MD, at University Hospital Southampton NHS Foundation Trust in Southampton, UK.
Media Inquiries
Greg Williams
Phone: 212-404-3500
Gregory.Williams@NYULangone.org