Your body regularly deals with cancerous areas through your immune system, so advanced screening and detection could lead to painful and expensive (but profitable) treatments that aren’t necessary. And could you imagine going through cancer treatment for an AI hallucination? There have been white coats saying people have cancer to treat and profit off of them when they did not. Of course, the white coats are responsible for harming people with unnecessary medications and vaccines that damage your immune system, not to mention the other OCGFC megacorps poisoning you in food and other products, your water… all to transfer your wealth to themselves, so they’re content to let you suffer, even unnecessarily. Also, all this unnecessary radiation can actually produce the cancer they’re looking for as well. And a few years ago hospitals were having doctors in India review these mammograms for cancer to save money, so would you trust an Indian doctor you didn’t even know was involved in your healthcare, as these white coats will harm or kill you.
https://www.cbc.ca/news/health/mammograms-ai-sweden-9.7067182
Swedish study of 100,000 women found AI-supported mammograms lowered rate of interval cancer by 12%
By Amina Zafar · CBC News
Some aggressive breast cancers can be difficult to detect and don’t always show up on mammograms, but a new study out of Sweden has found that artificial intelligence could help.
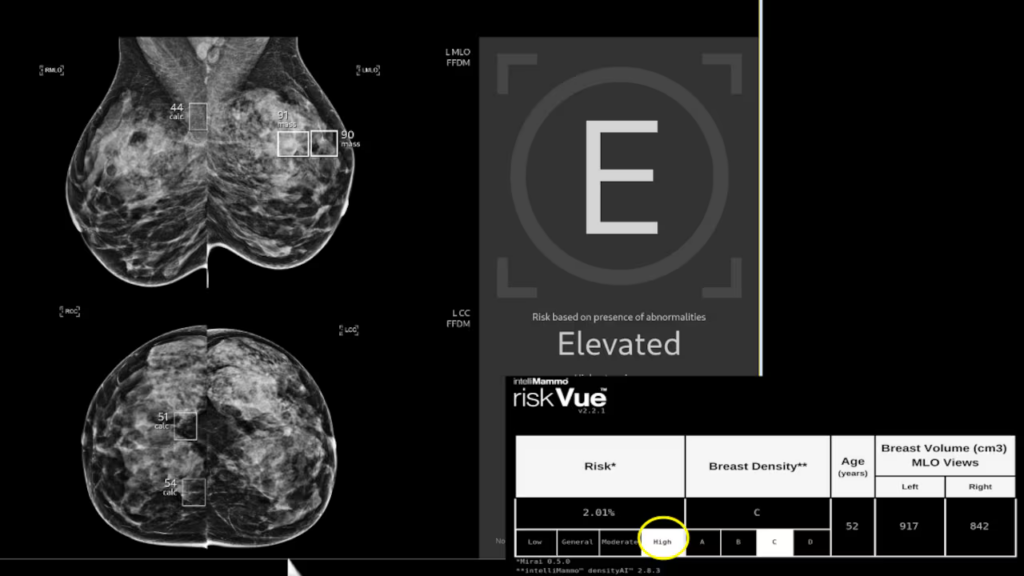
Mammograms are used to find breast cancers earlier, when they are easier to manage and treat. When radiologists used artificial intelligence to assist their readings, the rate of detection of breast cancers increased, resulting in fewer aggressive and advanced cases, a large trial in Sweden has found.
For the study — published in Thursday’s issue of the medical journal The Lancet — more than 100,000 women had mammography screenings. Half were supported by AI and the rest had their mammograms reviewed by two different radiologists, a standard practice in much of Europe known as double reading. It is not typically used in Canada, where usually one radiologist checks mammograms.
The study looked at the rates of interval cancer, the term doctors use for invasive tumours that appear between routine mammograms. They can be harder to detect and studies have shown that they are more likely to be aggressive with a poorer prognosis.
The rate of interval cancers decreased by 12 per cent in the groups where the AI screening was implemented, the study showed.
Lead author, Dr. Kristina Lång, said the large decrease was “a big sigh of relief.”
“The great outcomes we have seen [are] very promising,” said Lång, a breast radiologist and associate professor of diagnostic radiology at Lynn University in Malmo, Sweden.
Improving screening
In 2024, an estimated 30,500 Canadians were diagnosed with breast cancer, according to the Public Health Agency Canada, which also noted that the probability of surviving at least five years after diagnosis was about 89 per cent.
In 2024, the Canadian Task Force for Preventive Health Care said that mammograms shouldn’t be routinely offered to women under 50 who are of average risk, but noted that anyone 40 or over who wants a mammogram should be able to get one every two to three years. This practice hasn’t been widely adopted, though some Canadian provinces are moving toward that standard.
In Sweden, population-based breast cancer screening is offered to those between the ages of 40 to 74.
The frequency of screening also differs — in most Canadian jurisdictions, screening typically takes place every 24 months. In Sweden, it’s between 18 to 24 months.
Duration 2:03A new study suggests that artificial intelligence is showing major promise in detecting breast cancer, but researchers admit there are limitations. The technology can produce false positives — flagging too many mammograms as abnormal when there’s actually no cancer.
Throughout the two-year study, the mammograms that were supported by AI were triaged into two different groups. Those that were determined to be low risk needed only one radiologist to examine them, while those that were considered high risk required two.
The researchers reported that numerically, the AI-supported screening resulted in 11 fewer interval cancers than standard screening (82 versus 93, or 12 per cent).
“This is really a way to improve an overall screening test,” Lång said.
She acknowledged that while the study found a decrease in interval cancer, longer-term studies are needed to find out how AI-supported screening might impact mortality rates.
The screenings for the study all took place at one centre in Sweden, which the researchers acknowledged is a limitation. Another is that the race and ethnicity of the participants were not recorded.
The next step, Lång said, will be for Swedish researchers to determine cost-effectiveness.
AI could save public health dollars
Dr. Jean Seely, head of breast imaging at the Ottawa Hospital and a radiology professor at the University of Ottawa, says the value of AI-assisted mammograms is clear.
Seely, who was not involved with the study, noted that interval cancers are typically stage 3, which would mean treatment alone would cost more than $100,000 to $200,000 per patient.
“This is something that is not only saving lives, but saving public health dollars,” Seely said.
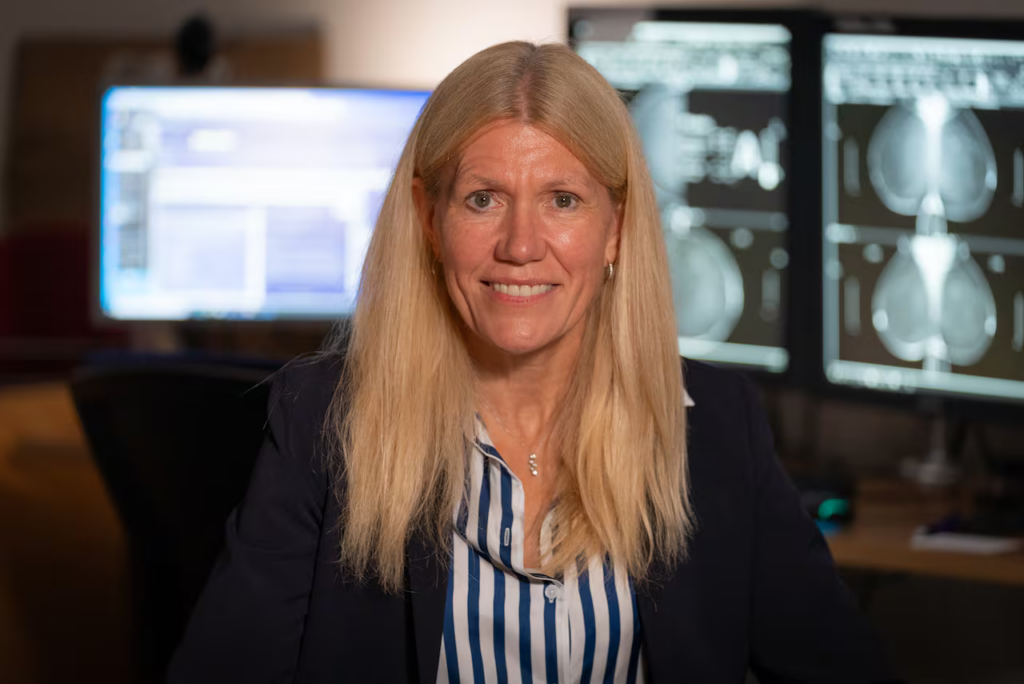
She’s used research funds to purchase AI software to help read mammograms.
“It’s like a double read and it helps me to focus my attention,” Seely said. “We’re all humans, right? We can sometimes be distracted.”
Investment in AI needed, oncologist says
Dr. Gerald Batist, a Montreal oncologist who was also not involved in the study, says there’s no longer a question that AI-supported mammography is a valuable tool.
His hospital, Montreal’s Jewish General, is currently weighing AI options for breast imaging.
“We should be investing in AI solutions,” Batist said. “These studies confirm that they pick up things that … the human eye doesn’t see.”
As for what’s next, Batist called on health ministers to talk to their counterparts in charge of innovation and technology.
“Health care and regulators have to move at the speed of cancer, not at the speed of bureaucracy,” he said.